What is Osteoathritis?
Between all our joints we have protective tissue called cartilage which primarily acts as a shock absorber for movement. Over its life this cartilage goes through a constant process of wear and repair – this is a normal process. However, sometimes the repair process slows down and cannot keep up with the wear process and over time this leads to a loss in cartilage. This results in a loss of joint space and over many years leads to structural changes in the joint.
Why does this happen?
There are several factors that play a role in the acceleration of Osteoarthritis:
- Trauma – this might be from an injury within the joint space or a surgery. We now know that when there is a bleed in the joint space either as a of result of a trauma or surgery this disrupts the cartilage turn over process.
- Genetics – all our cells have a time clock and for some of us that influences the wear and repair ability of cartilage in our joints.
- Obesity – When we carry additional weight, our joints must work harder to carry that additional load. That extra weight means we move less and therefore are not as strong around our joints so the joint does not receive efficient load. This means that repair process is not optimised. Additionally, when we are overweight, that additional fatty tissue means we are living in a chronic state of inflammation. Some early science shows us that that persisting inflammation in the blood from diet, weight and even stress affects the repair process of our cartilage.
But if my joints are ‘wearing’ then what can I do?
So, we can’t grow that cartilage back, but the good news is there is a lot you can do to help maintain and optimise the joint and the environment in which it lives, even in the most severe cases.
- Getting moving – regular, quality, strength exercise helps to lubricate the joint and stimulates the repair process of the remaining cartilage. By keeping our muscles strong and enduring, the joint can then work more efficiently in our everyday activities. This is often where physio can help to tailor a bespoke strength and movement programme to help your joint on its way.
- Eating a healthy, varied diet – fuelling our bodies well gives our muscles, joints and cartilage the necessary nutrients they need to promote that repair process. Ensuring we minimise pro-inflammatory foods i.e. ultra-processed foods, alcohol, sugars.
- Sleep – if our bodies and brains are not rested and restored then we lack the motivation and energy to put regular exercise into our day. Ensuring you get a consolidated chunk of sleep is important, between 5-10 hours.
- Weight management – by improving your baseline weight you then will reduce systemic inflammation, have more energy, move better and therefore load your joint more efficiently.
But I keep active – I never stop moving so why do my joints hurt?
Well, keeping active is great for lots of reasons, from your heart and lung health to your mental well-being. However, there is a difference between being active and being strong and enduring. Our joints can only give us what we given them, and health guidelines recommend 150 minutes of targeted exercise per week with a mixture of cardiovascular and resistance training.
Once we become sore, we often avoid normal regular movements, or we continue moving but not well. If this cycle persists then the overall efficiency and endurance of the joint and muscles will drop. This makes it feel like our joint is worsening but it hasn’t, it’s just lost tolerance. We end up in a viscous cycle.
This is where good pain management is important to sustain quality and regular exercise.
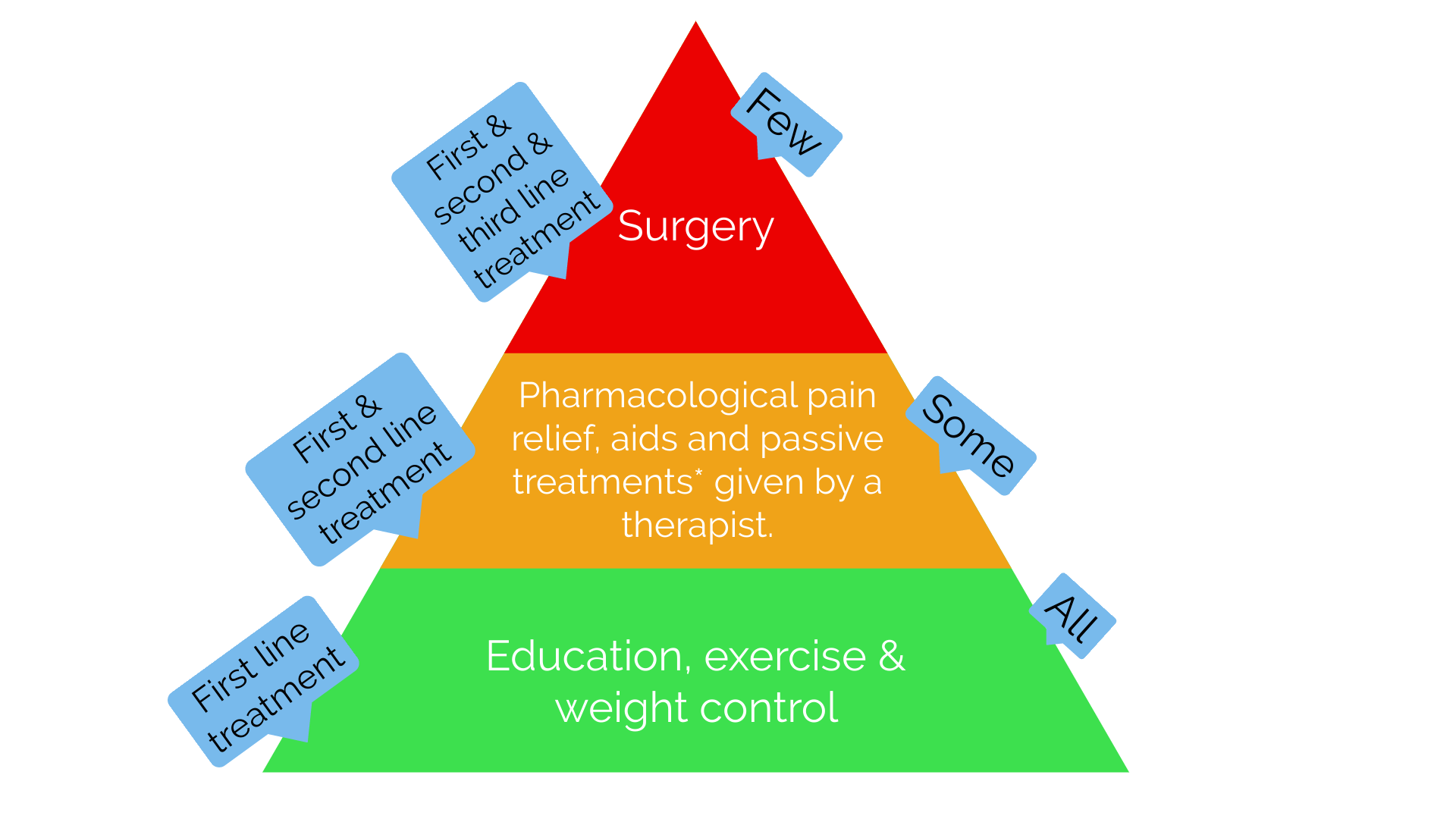
What pain management options do I have?
- Anti-inflammatories – either topical or oral anti-inflammatories can be very effective for a few days in acutely painful episodes e.g ibuprofen or voltarol rub (please check with pharmacist that you can take these).
- Bracing – this can sometimes be a useful adjunct to offload the joint and enable you to move with less pain and therefore get stronger.
- Corticol steroid injections – This is a last resort pain relief option used by GP’s or Orthopaedic doctors to deliver anti-inflammatory directly to the painful site. This works well particularly if the soft tissue is inflamed but is not a long-term solution to the overall picture. There is mixed evidence of its efficacy and should be utilised in combination with lifestyle changes. Corticol steroids can also weaken the ligaments and tendons they are injected into, therefore a good shared decision-making discussion about risks versus benefits must be had with your Doctor.
- Surgery – the point at which you are looking down the surgical route is usually when you have exhausted all the above management options (see diagram below) and despite this your function is declining and pain is increasing.
If you would like more information please contact our reception to book an appointment with one of our highly skilled physiotherapists or to reserve a place at our upcoming patient information talk at 11am on Wednesday 13th March: ‘Knee Osteoarthritis: treatment and management options’
e: reception@cranfoldphysio.co.uk
t: 01482267747
Write a comment:
You must be logged in to post a comment.